Insulin

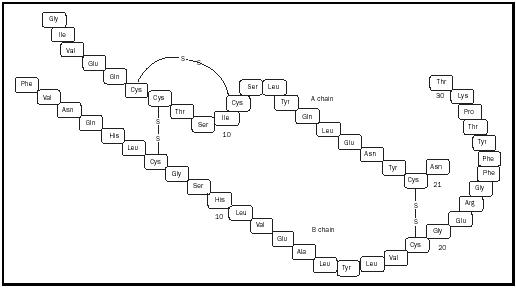
Insulin is a small peptide (protein) consisting of fifty-one amino acids synthesized and stored within the pancreas, an organ situated behind the stomach. The protein itself consists of two chains, denoted A and B, linked by disulfide (sulfur-sulfur) bridges between cysteine residues (see Figure 1).
Insulin is a hormone, a chemical transported in the blood that controls and regulates the activity of certain cells or organs in the body. When blood sugar levels rise following a meal, the pancreas is stimulated to release insulin into the bloodstream. In order for tissues to absorb glucose from the blood, they must first bind insulin. Glucose metabolism is necessary for cell growth and energy needs associated with cell function. When insulin binds to receptors on cell membranes, glucose transporter proteins are released from within the cell to the surface of the cell membrane. Once on the exterior surface of cells, glucose transporters can carry sugar from the blood into the tissue where it is metabolized. Without insulin, cells cannot absorb glucose and effectively starve.
A deficiency in insulin production results in a condition called diabetes mellitus. Approximately 6.2 percent of the population in the United States is affected with diabetes. Type 1 diabetics account for 10 percent of those individuals suffering from diabetes mellitus. It is also known as juvenile diabetes and generally develops in young people, typically between the ages of ten and fifteen years, as a result of an autoimmune disorder. Why the body's immune system turns on itself, attacking and destroying beta cells, the pancreatic cells in which insulin is synthesized, is not clear. The unfortunate consequence is insulin deficiency.
The majority of individuals afflicted with diabetes mellitus suffer from type 2 diabetes. The onset of type 2 diabetes occurs much later than for type 1 and typically in people over the age of fifty. The pancreas of type 2 diabetics continues to produce and release insulin. However, cells do not respond appropriately to insulin levels in the blood. This condition is known as insulin-resistance and is associated with obesity and high blood pressure. Children who are obese can also develop type 2 diabetes.
Gestational diabetes affects 3 to 5 percent of pregnant women. Onset generally occurs in the fifth or sixth month of pregnancy. In pregnant women, the placenta produces hormones to support the growing fetus. Some of these hormones (e.g., estrogen and cortisol) interfere with the actions of insulin. Insulin-resistance develops despite adequate blood insulin levels. Gestational diabetes does not last beyond pregnancy and the condition disappears after delivery.
Before the discovery of insulin, type 1 diabetics usually died within a few years of onset of the disease. During the early 1920s, a young Canadian physician, Frederick Grant Banting, working with John James Rickard Macleod, professor of physiology at the University of Toronto, and Charles Best, a medical student, discovered insulin while performing investigations on extracts acquired from dog pancreas. Soon after, Banting and Macleod were awarded the 1923 Nobel Prize in physiology or medicine for their discovery (Banting reportedly split his share of the prize money with Best).
Insulin was rapidly put into clinical use, chiefly through the efforts of August Krogh, a Danish scientist who cofounded the Nordic Insulin Laboratory in Copenhagen, Denmark, for the production of insulin. Large quantities of insulin were initially acquired from the pancreatic tissues of slaughtered animals, typically cows and pigs. Although bovine (cow) and porcine (pig) insulin are still the major components of commercially available insulin in the United States, the use of human insulin preparations is rapidly growing. Since the 1980s, recombinant DNA techniques have made human insulin available for clinical use. Genetically modified strains of Escherichia coli bacteria or Saccharomyces cerevisiae (baker's yeast) containing human genes coding for insulin have been developed for the mass production of human insulin.
Insulin is not a cure for diabetes. It does, however, allow diabetics, especially those with type 1 diabetes, to gain some control over their condition. Insulin is typically administered by subcutaneous (under the skin) injection. There are four principal types of insulin preparations commercially available. Insulin lispro (ultra-short-acting insulin) is rapidly absorbed into the blood and lasts only 3 to 4 hours. Regular insulin, on the other hand, takes 30 minutes to become effective, and lasts 5 to 7 hours. Lente and NPH (neutral protamine Hagedorn) insulin preparations are longeracting formulations typically administered every 12 hours. Finally, mixtures of insulin preparations are also commercially available. Typical mixtures consist of 70 percent NPH and 30 percent insulin lispro.
SEE ALSO Genetic Engineering ; Glycolysis .
Nanette M. Wachter
Bibliography
Dewitt, Dawn E. and Hirsh, Irl B. (2003). "Outpatient Insulin Therapy in Type 1 and Type 2 Diabetes Mellitus: Scientific Review." Journal of the American Medical Association 289(17):2254–2264.
Katzung, Bertram G. (1998). Basic & Clinical Pharmacology, 7th edition. Stamford, CT: Appleton & Lange.
Internet Resources
National Institute of Diabetes & Digestive & Kidney Diseases of the National Institutes of Health. Available from http://www.niddk.nih.gov .
Nobel Foundation E-Museum. "The Nobel Prize in Physiology or Medicine 1923." Available from http://www.nobel.se .
Comment about this article, ask questions, or add new information about this topic: